I wanted to reflect on the two days I had at hospital just before we broke up for the summer holiday as it was quite an insightful taster into what my third year of medicine may involve.
Soo...I woke up super early at about 6ish which was not part of my normal house bound uni routine. Got ready, ate two bananas and the rest of my innocent smoothie and headed out at around 7.30. On my way out I did miss the first bus but thankfully another one came shortly after. The next bus also did not take too long to arrive. Seven minutes later I was at the hospital. I was a little lost on my way to the education centre which is far out away from the main hospital buildings so I asked around a few staff who were on their way to their shift who seemed to know the hospital well for directions and I was guided to the right building. I overcame the first step of actually finding the right building 😅 and I made it thirty minutes before the start which is good.
As I entered the building the coordinator gave me some instructions for the day and I made my way up to the lecture theatre where there was a handful of people. There was already a girl signing her name and I introduced myself. I then took a sit nearby a friend I knew and we chatted and I got to know the new person I had just met. Then we got a brief introduction into how third year will be like.
Then we got split up into two big groups. The first group stayed in the lecture room and the rest went to a nearby building with a teaching ward (with no actual patients). Our clinical teaching fellows (CTFs) split us up into two smaller groups where we sat round a table and discussed within the group some professionalism cases. Then we swapped and went to the other side of the room to have a sort of Q&A session with a third year medical student and a CTF about what life in third year will be like which was very insightful.
Then we went to the ‘fake wards’ where another CTF gave a presentation on the journey of a patient from arrival to A&E through triage and being referred to the right service/department. As well as discussing the different teams that will be involved in the patients care.
We then got to have some practise on a Sim Man which is essentially used to replicate a patient as this dummy has been made to simulate a humans pulse, breathing, eye opening and closing. So we got to listen to the ‘patients’ lungs using our stethoscopes, feel for the pulses as well as observe the chest expansion. The sims man was also connected to an ecg and has his heart rate and blood pressure monitored.
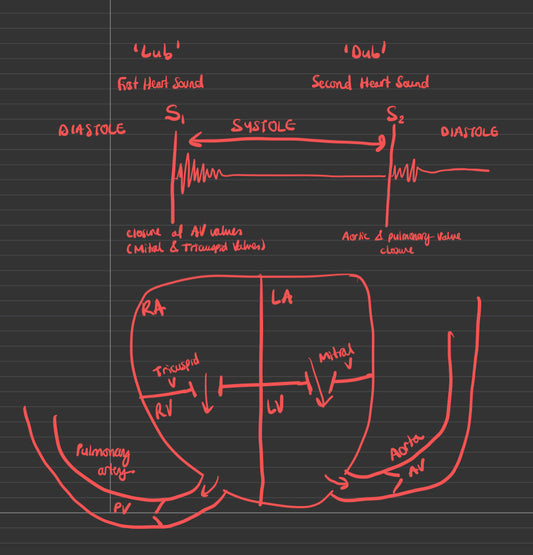
On the second day of our hospital orientation, we started by learning about heart sounds with one of the CTFs. We used our stethoscopes to listen for normal heart sounds and abnormal heart sounds i.e. heart murmurs from a heart and lung sound simulator tool. We were then quizzed on the various heart sound abnormalities we heard and were asked to describe the murmurs and when they occurred relative to S1 (closure of atrioventricular valves) and S2 (closure of aortic and pulmonary valves).

We then practised clinical examination skills with a partner. We carried out a few tests to be able to calculate a NEWS (National Early Warning score) that is often used to monitor a patient current physiological status. This is often carried out by nurses on the bedside a few times a day and is an easy way for them to be alerted to any patient who is deteriorating and inform the doctor for early interventions need to ensure the patient is stable. Having very limited practical experience due to the covid-19 disruption I was pleasantly surprised that I got an accurate reading of my peer's blood pressure manually after checking with the electronic blood pressure monitor. I then proceeded to take my peers pulse, respiratory rate and oxygen saturation.
After lunch we were split into different departments. I was placed in the geriatrics ward. The registrar in charge of this ward gave as a brief tour, as you first enter the hall there is a storage room with medical supplies. On the opposite side there were two isolation rooms which were occupied with tuberculosis positive patients. The registrar explained that although this was a geriatrics ward, patients' age vary and a lot of the patients are in the ward due to chronic conditions. Since it was the afternoon and ward rounds already occurred in the morning the registrar went through a couple of the patients history with us from the computer in the staff room as another ward round may make the patients unsettled.
There was some interesting and quite sad patient cases. One case that stood out to me was that of a middle aged patient with very progressive Parkinson's disease with limited mobility but no effective treatment. This was quite touching and one where the multidisciplinary team would need to discuss their management clearly with the patient and their family.
This then lead onto a brief discussion on "Do Not Attempt Resucistation -DNAR" orders. This is a very complex matter whereby ensuring to take all aspects of the case into consideration is vital including the legal requirements. After this discussion, our day came to a close!


![Remnote: Best Note-Taking App and Spaced Repitition Tool [medical student]](http://perseveringmedic.co.uk/cdn/shop/articles/Website_images-4.png?v=1657633666&width=533)